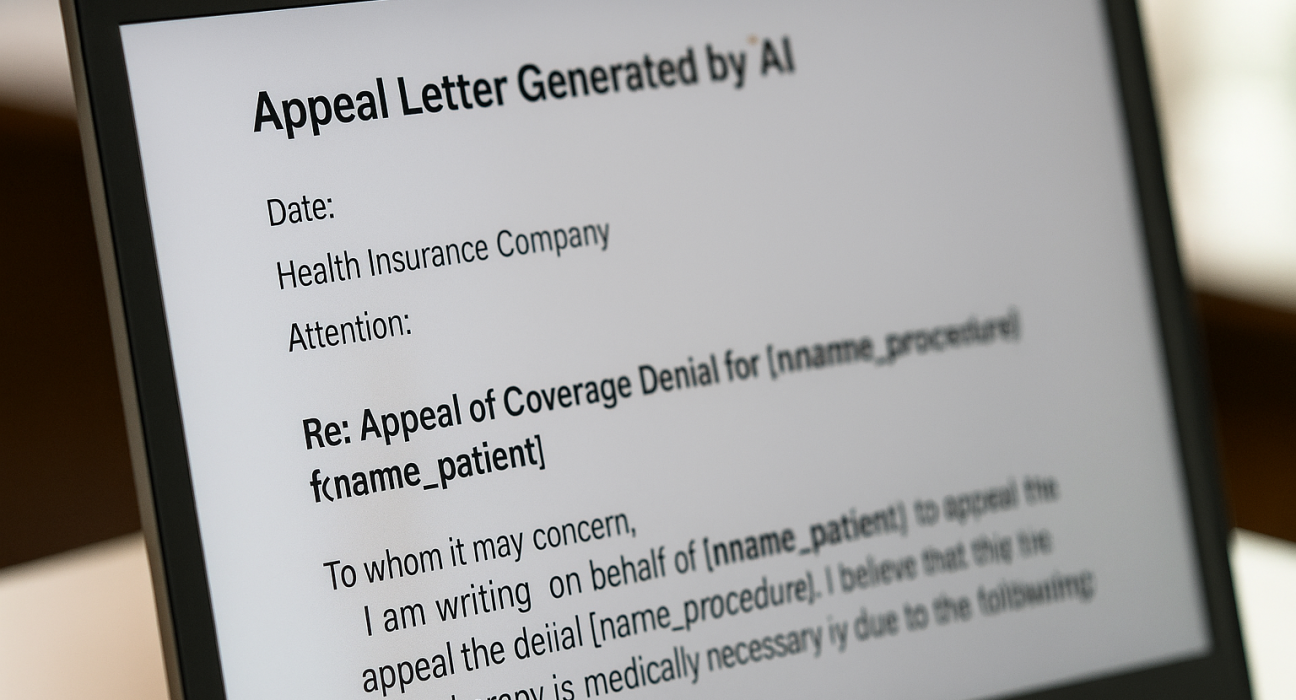
A Research Triangle Park–based startup, Counterforce Health, has developed an AI tool to help patients and clinics appeal health insurance denials. The platform—which is free for patients and caregivers—is gaining traction with healthcare providers like Wilmington Health. It automatically drafts appeals letters by analyzing insurance policies, denial letters, and medical records, drawing on medical journals and review guidelines to build compelling, evidence-based arguments. The AI system reportedly achieves up to a 70% success rate, significantly reducing time spent on appeals.
billingparadise.com
Key Insights
- AI vs AI: Founded by Neal Shah, Counterforce aims to level the playing field against insurers that increasingly rely on automated systems to deny claims.
ProgramBusiness - Accessibility & Outreach: Beyond its digital platform, Counterforce operates Appeals on Wheels, a mobile clinic bringing AI assistance to rural areas with limited internet.
Counterforce Health - Efficiency Gains: Health professionals report the tool can process multiple denials in a couple of hours—transforming appeals that once took days into minutes.
https://www.wect.com - Systemic Impact: With denial rates rising (e.g., 20% of ACA claims denied in 2023), these AI tools address a critical bottleneck in healthcare access.
Investopedia
Future Projections
| Area | Outlook |
|---|---|
| Patient Empowerment | Wider adoption may lead to higher appeal success rates and reduced emotional stress for patients. |
| Institutional Adoption | Clinics—and potentially insurers—may integrate AI tools for faster dispute resolution. |
| Regulatory Focus | With AI increasingly used in denials, stronger regulatory oversight may emerge to ensure fairness and accountability. |
| Axios | |
| Innovation Catalyst | Counterforce’s model could inspire broader healthcare justice innovations—embedding AI in policy, legal, and workflow improvements. |
Neutral Reflection
Counterforce Health exemplifies a growing trend of using AI to counterbalance system-level inequities—this time in healthcare. While insurers’ automation can limit patient access, Counterforce’s platform not only streamlines appeal processes but also provides meaningful legal and research support. By combining technology, advocacy, and accessibility, it offers a promising path to more equitable healthcare outcomes. As use widens, ensuring transparency, human oversight, and data privacy will be key.
Let me know if you’d like a condensed summary, process visualization, or comparisons with other AI-assisted appeals tools.






Leave feedback about this
You must be logged in to post a comment.